MANAGING DIABETES
So many medicines—what do I need to know?

Let’s take a closer look at insulin and non‑insulin treatments for type 2 diabetes, including GLP‑1 receptor agonists.
Many people with type 2 diabetes will need to combine healthy eating and physical activity (such as walking) with 1 or more medications. There are 2 classes of diabetes medication that we talk about: non-insulin and insulin. Both are taken to help keep blood glucoseBlood glucoseThe main sugar found in the blood, and the body’s main source of energy. within the target range. Some diabetes medications are taken orally (pills), and some are by injection.
Your health care professional will let you know if you need to add medicine to your diabetes care plan. This is called “treatment intensification.” They will also let you know if and when it’s time to change your medicine if your diabetes has changed.
Oral antidiabetic drugs (OADs)
There are many types of OADs. They work in different ways to lower blood glucose. Some commonly used classes include:
- Metformin (biguanide)
Helps lower insulin resistance and reduce the production of glucose - Sodium-glucose cotransporter-2 or SGLT-2 inhibitors (dapagliflozin, empagliflozin, canagliflozin, ertugliflozin)
Help the kidneys to get rid of extra glucose in the body through the urine - DPP-4 inhibitors (sitagliptin, saxagliptin, linagliptin, alogliptin)
Help prevent the breakdown of GLP-1, a hormone produced in the intestines - Thiazolidinediones or TZDs (pioglitazone, rosiglitazone)
Help improve the liver, muscle, and fat cells’ response to insulin, meaning more glucose leaves the blood and enters the muscles and fat (where it belongs) - Sulfonylureas (glimepiride, glyburide, glipizide)
Help the pancreas to release more insulin
OAD combinations
Since the different kinds of OADs help lower blood glucose in different ways, some may be used together. These options allow health care professionals to come up with treatment plans that meet individual needs.
GLP-1 receptor agonists
Your health care professional may also prescribe a GLP-1 receptor agonist (GLP‑1 RA) as part of your therapy.
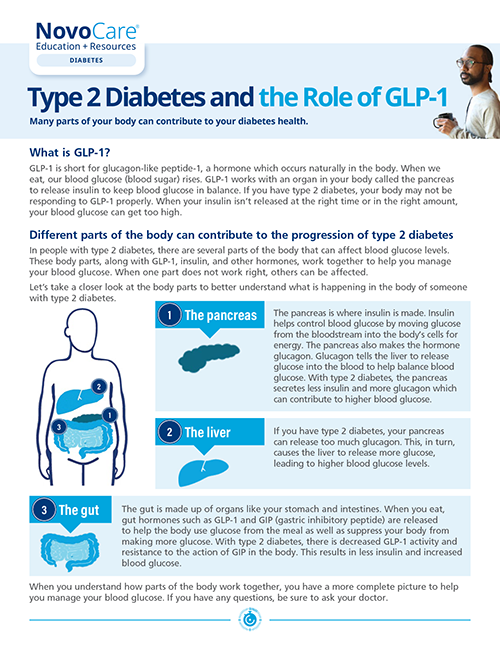
GLP-1 is short for glucagon-like peptide-1. It's a naturally occurring hormone released from cells in your body that helps it release insulin to help keep blood glucose in balance. If you have type 2 diabetes, your body may not be responding to GLP-1 properly. When your insulin isn't released at the right time or in the right amount, your blood glucose can get too high.
A GLP-1 RA is a non-insulin medicine that acts like the GLP-1 in your body. These medicines work by:
- Helping the pancreas release more insulin after you've eaten
- Telling the liver not to release so much glucose at mealtimes
- Slowing down digestion of food so after-meal blood glucose levels don't rise as high
GIP/GLP-1 receptor agonists
A GIP/GLP-1 receptor agonist (GIP/GLP-1 RA) medication is one that has the actions of GLP-1 listed above and also mimics GIP (gastric inhibitory peptide), another naturally occurring hormone. This type of medicine also helps your body release insulin in response to meals.
Amylin agonists
Another option your doctor may prescribe is an amylin agonist. This is an injectable drug that acts like a hormone produced by the pancreas. It affects several different organ systems and works by:
- Slowing down the movement of food leaving the stomach and prompting an end to eating through the feeling of being full
- Telling the liver not to make so much glucose at mealtimes
The insulinInsulinA hormone made by the beta cells in the pancreas that helps glucose move from the blood into the cells. Insulin is also an injectable medicine that is used to treat diabetes by controlling the level of glucose in the blood. that your body makes naturally is a hormone that is important for producing energy from food. Some people with type 2 diabetes may not be able to use their own insulin well. This is called insulin resistance. It causes blood glucose levels to increase.
As diabetes changes over time, the body makes less insulin and can’t control blood glucose levels. For these people, insulin can be injected under the skin. This helps lower blood glucose levels back to their normal range.
Different insulin medicines work in different ways to replace the insulin you’re missing. They are grouped together based on:

- When they start to work (onset)
- When they have the greatest effect on blood glucose (peak)
- How long they work (duration)
Ways to describe insulin medicine
Human insulin
Human insulin is actually made in a lab. It’s called “human” because the structure is identical to the insulin your body makes.
There are 3 types of human insulin:
- Short-acting. This insulin, also called regular insulin, is usually taken 30 minutes before a meal and lasts 3 to 6 hours.
- Intermediate-acting. This type of human insulin, also called NPH insulin, is taken 30 minutes before breakfast, before the evening meal, or at bedtime, and is effective for anywhere from 12 to 18 hours.
- Premixed. This type of human insulin includes both a regular insulin and an intermediate-acting insulin. It is taken 30 minutes before breakfast and/or the evening meal and works for anywhere from 10 to 18 hours.
Insulin analogs
Insulin analogs are human insulin with small changes made to the hormone so that it is absorbed faster or lasts longer in the body.
The 3 main types of insulin analogs are:

- Long-acting. Also called basal insulinBasal insulinA type of injected insulin that is absorbed slowly and starts to lower blood glucose. There are 2 types of basal insulin: Daily and weekly. Daily basal insulin begins to work within 4 to 6 hours after injection. Its strongest effect is 10 to 18 hours after injection depending on the product. This gives the body a low level of insulin to manage blood glucose between meals and overnight., this type is not taken with food. It works slowly and lasts longer to control blood glucose between meals and when you sleep. Basal insulin can be taken less frequently than other types of insulin.
- Fast-acting. Also called bolus insulin. Depending on the medicine, this type of insulin may be taken just before a meal, at mealtime, or shortly after starting a meal.

- Premixed. This type is a mixture of fast‑acting and intermediate-acting insulins. It works to control blood glucose at mealtime and works anywhere from 16 to 24 hours.
Each type of insulin helps manage blood glucose. But no one type is right for everyone. Each person’s insulin need is different and may change over time. Your health care professional will prescribe the insulin that is best for you. And, as treatments and medication options continue to evolve, it's important to check in with your health care team on what the best options are for you.