Managing your type 2 diabetes with insulin
A guide to how insulin may help you reach the diabetes goals you’ve set with your health care professional.

Actor portrayals.

Actor portrayals.
About diabetes
What is diabetes?
Diabetes is a condition where your body doesn’t make enough insulin, makes no insulin at all, or doesn’t respond to insulin properly.
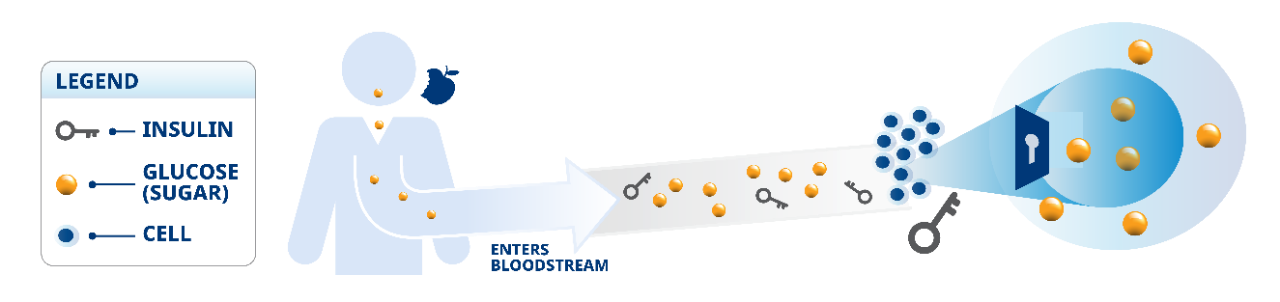
What is insulin and how is it used in the body?
- The insulin your body makes naturally is a hormone that helps the body use glucose
- The body turns the food you eat into glucose
- As blood glucose rises, the body releases more insulin
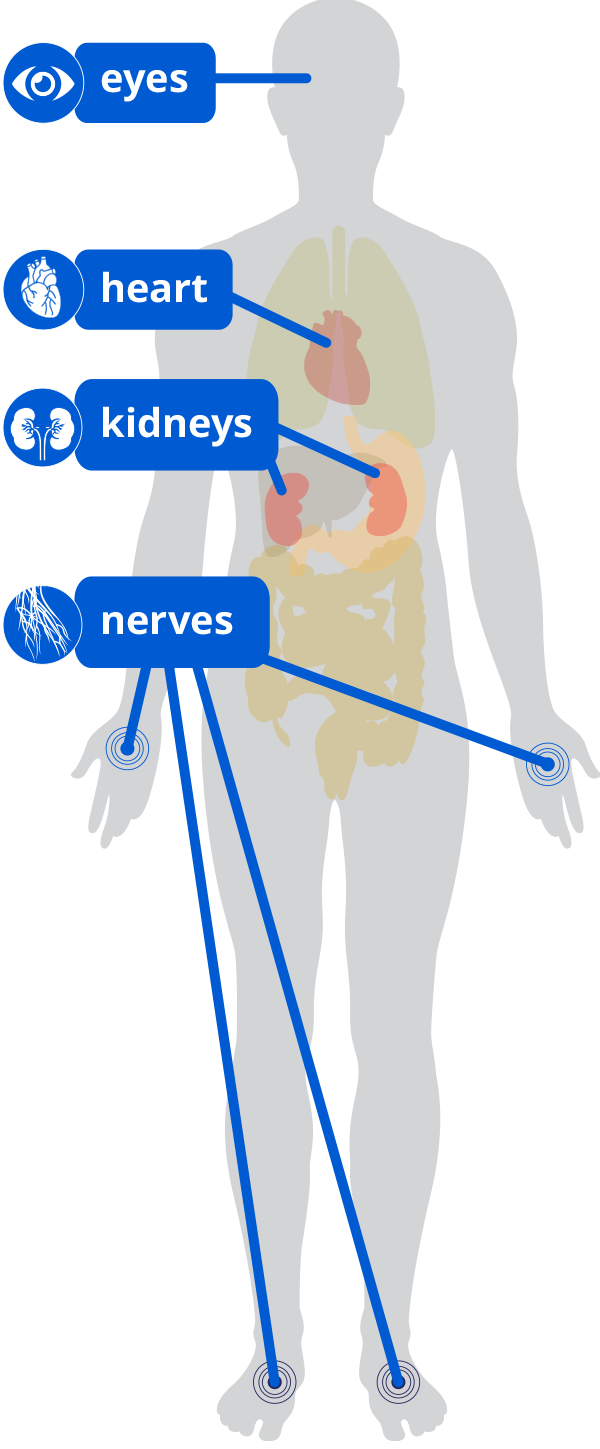
Uncontrolled diabetes may lead to other related health problems.
- When you have high blood glucose (sugar) for a long time, you have a greater risk of developing diabetes-related problems (also called ”complications“)
- These may include complications that affect:
— Heart (cardiovascular disease)
— Nerves (neuropathy)
— Eyes (retinopathy)
— Kidneys (nephropathy)
Managing the long-term risks of diabetes:
The long-term damage that diabetes can cause may not show up for several years. Even then, the signs may be so small that you don’t notice them.
It’s important to understand your risks with diabetes and its long-term complications. Talk to your health care professional about what this means for you.
38.4 million people in the United States have diabetes.
And the number is growing. This number includes both type 1 and type 2 diabetes.
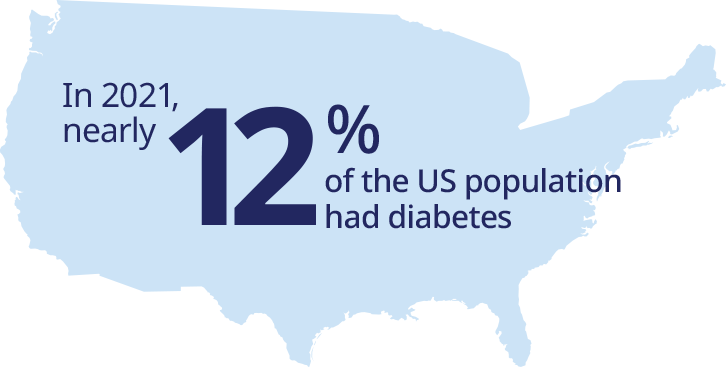
Diabetes is a global epidemic:
It’s estimated that 578 million people worldwide will have diabetes by 2030.

Actor portrayals.
Understanding blood glucose management


Actor portrayal.
A1C
is the primary tool and most widely accepted blood glucose measurement. The test measures average blood glucose levels over the past 2 to 3 months and may give you an idea of how well your overall diabetes care plan is working.
FPG
is your “fasting plasma glucose,” or your blood glucose when you have been “fasting” (not eating, or drinking, except for water) for at least 8 hours. Typically, you check this in the morning when you wake up.
TIR
is “Time in Range.” This is the amount of time you spend in your target blood glucose range. For most people, this is between 70 and 180 mg/dL.a
aTalk to your health care professional about what your personal blood glucose goals should be.
Remember:
Blood glucose rises right after eating, so check your blood glucose regularly before and after meals to see how certain foods affect your levels.
Even if you have been trying to do everything you can to manage your diabetes, you may find that you are no longer reaching your A1C goal.
Diabetes changes over time and may get more difficult to manage.
Getting your blood glucose under control is the goal of your diabetes care plan and may also reduce the risk of some diabetes-related problems.
In fact, the American Diabetes Association says that lowering your A1C to less than 7% may help reduce the risk of some diabetes-related complications.a
How your A1C and blood glucose are related
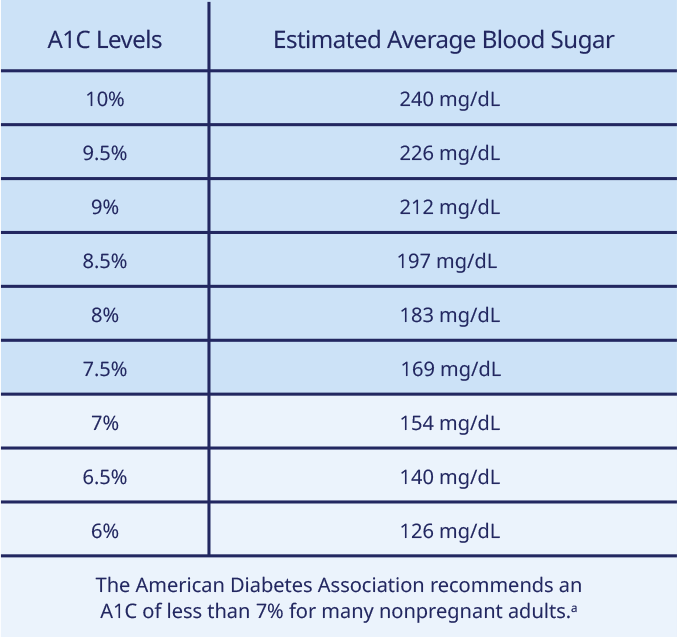
aYour A1C goal may be higher or lower than the ADA recommends. Ask your health care professional for your specific goal.

Actor portrayals.
Types of insulin
Diabetes changes over time, and your medicine may need to change too.
- You may have started out treating your diabetes with lifestyle changes (diet and physical activity) and pills (oral antidiabetic medications, eg, metformin)
- You may get to a point where diabetes pills don’t adequately manage your diabetes. If so, you may be prescribed some types of insulin such as a long-acting (basal) insulin in the morning/night with or without bolus (rapid or short-acting) insulin around meals
- Many people with type 2 diabetes currently taking long-acting (basal) insulin may need additional control at mealtimesa
aTalk to your health care professional about how insulin may help you achieve your blood glucose (sugar) goals.

Actor portrayals.
Starting insulin may feel overwhelming, but it’s the most natural and effective treatment for diabetes.
Insulin therapy mimics the body's normal insulin patterns throughout the day.
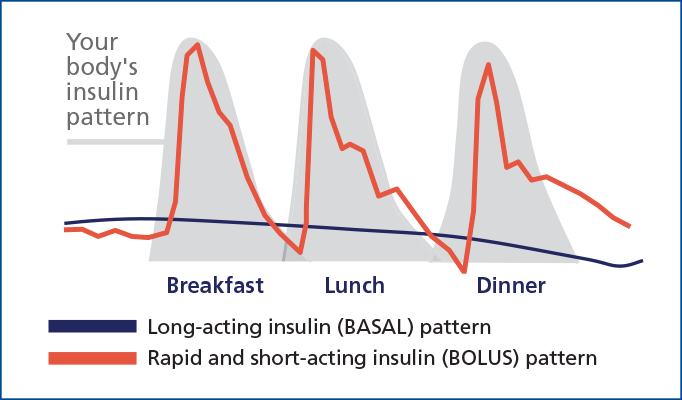
Long-acting insulin (basal):
Insulin that is taken once daily and absorbed slowly to mimic the body’s natural release of insulin and provide even blood glucose (sugar) control.
Mealtime insulin (bolus):
Known as rapid and short-acting insulin because it helps control blood glucose spikes caused by eating.
Basal-Bolus:
A treatment regimen that acts like the body’s normal insulin patterns throughout the day by using both long-acting and rapid or short-acting insulin together.
aTalk to your health care professional about how insulin may help you achieve your A1C goals.

Actor portrayals.
Because diabetes changes over time, your medication may have to as well.
You may be ready for long-acting (basal) insulin if:
- Your diabetes medication is no longer helping you reach your blood glucose and A1C goals
- Your body doesn’t respond well to your naturally occurring insulin
- Your body doesn’t produce enough or any insulin
Diabetes is a progressive condition
It’s important not to feel defeated by changing conditions that may need a medication change. Remember, you have options and long-acting (basal) insulin may be a solution to help you manage your blood glucose.
aTalk to your health care professional about how insulin may help you achieve your blood glucose goals.

Actor portrayals.
It may, if you are taking long-acting insulin and are either:
- At your fasting blood glucose goal, but not reaching your A1C goal
- Your long-acting (basal) insulin dose is greater than 0.5 units/kg/day of your body weight
It may be time to make a change. And you are not alone!
If long-acting (basal) insulin isn’t helping you reach your target A1C goal,a mealtime insulin may be prescribed. Adding more insulin over time does not mean failure. Think of it as another way to manage your diabetes and meet your A1C goal.
aTalk to your health care professional about how insulin may help you achieve your blood glucose (sugar) goals.

Actor portrayals.
Your blood glucose rises after eating.
Assuming you eat 3 meals a day, you can spend up to 12 hours, or 50% of your day, with higher-than-normal blood glucose.
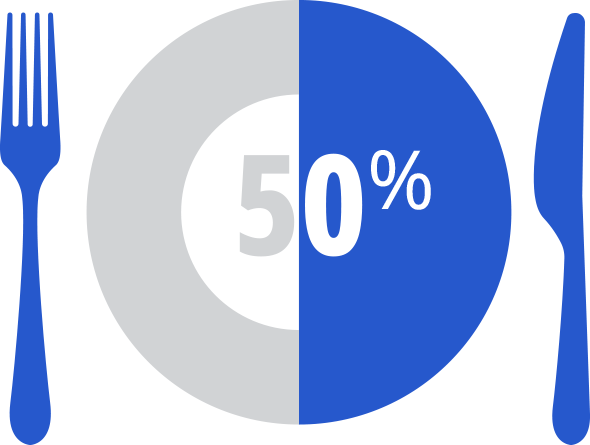
In basal-bolus therapy, up to 50% or more of your daily insulin may eventually be rapid or short-acting, therefore:
- Your diabetes care team may need to add rapid or short-acting insulin to 1 or more meals
- Or adjust your basal-to-bolus insulin ratio to help you reach your goals
Getting results involves taking your medicine as prescribed.
Tips for taking
mealtime insulin:

Keep your insulin in the kitchen (refer to each product’s storage information)

Carry your pen and needles, or vial and syringe, with you at all times

Set reminders and/or alarms on your cell phone, or write them in a planner
Tips for taking
long-acting insulin:

Pair your injection with a daily habit like brushing your teeth or drinking your morning coffee

Set reminders on your smartwatch, cell phone, or with a digital assistant

Ask a family member or friend to help you remember or check in with you

Actor portrayals.
Looking for additional support? Sign upa for a Diabetes Health Coachb today
aBy clicking the link above, you are leaving the NovoCare® website
bEligible for commercially insured patients only. Not available to patients with Medicare or without commercial insurance.

Actor portrayals.
Making insulin part of your life

Here are some common concerns and answers that may help you better understand the changes in your care plan.
“I don't want to have to change my life to fit my insulin!”
With help from your HCP, your insulin dose may be adjusted and tailored to your activity and eating patterns
“I stopped taking my insulin because I feel noticeably better.”
Even if you feel better, you should not just stop taking your insulin. Insulin is an ongoing treatment; it is not a quick fix or a cure. Talk to your health care professional about your individual treatment routine
“I only take my insulin when I feel sick.“
Some medicines are given to you only when you feel sick, while other types of medicines should be taken regularly. However, insulin needs to be taken only as prescribed for it to help safely and effectively manage your diabetes. You cannot always tell whether your blood glucose (sugar) is high or not, so it’s important to continue to check your blood glucose, take your insulin as prescribed, and speak with your health care professional about any questions or concerns you may have
“I’m worried about low blood sugar.”
Low blood glucose is a possible side effect of all insulin, and even some non-insulin medicines. Taking your insulin as prescribed is the best way to help manage your blood glucose
Be patient and keep at it—diabetes management is a marathon, not a sprint!
Insulin is not a quick fix or a temporary solution; even after your A1C improves, you will still need to take your insulin and other medications to stay at goal.
Changing your A1C will probably take longer—think of it as a snapshot of your blood glucose (sugar) control over the last 2 to 3 months.

Actor portrayals.
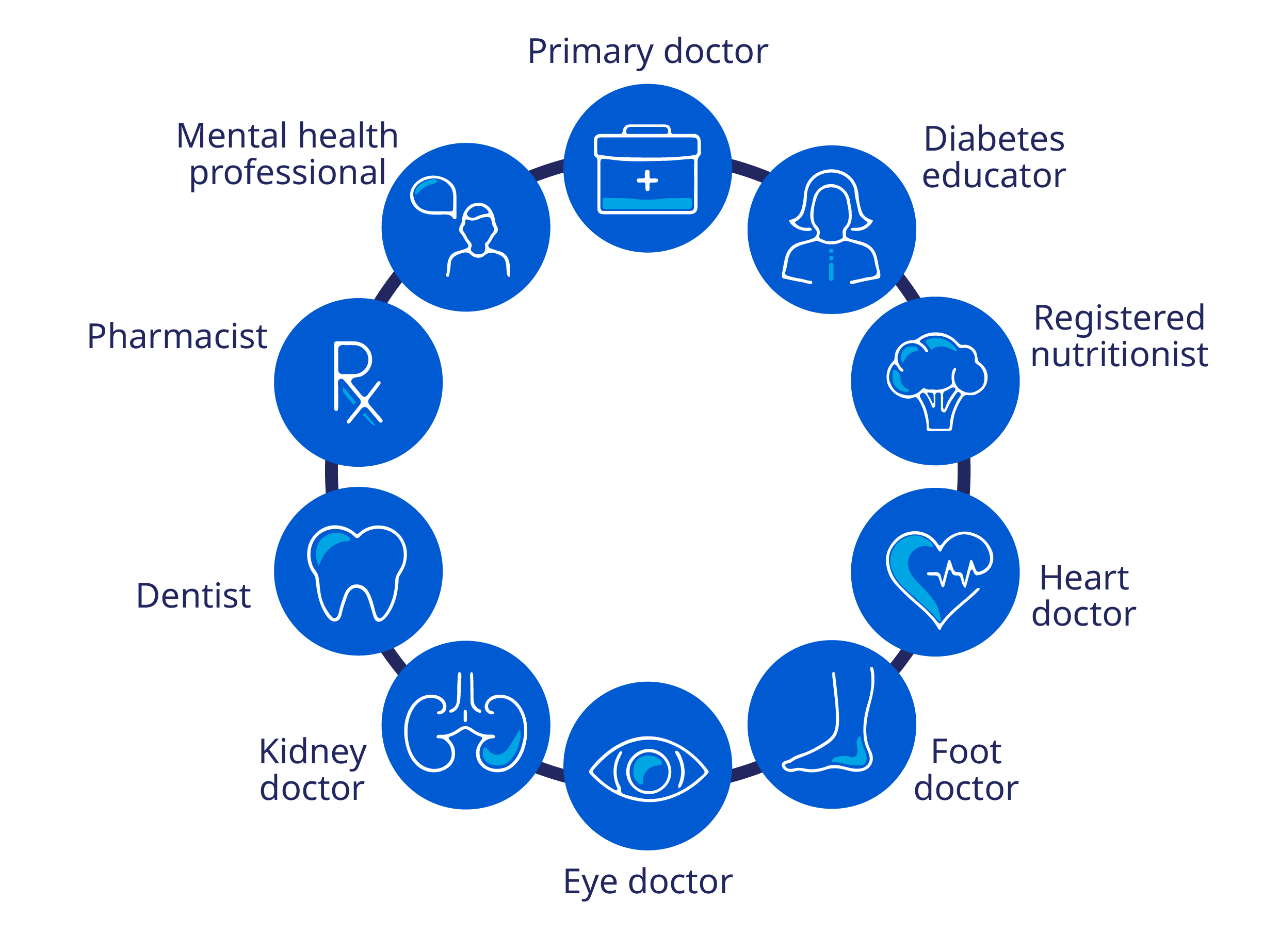
Work closely with the members of your diabetes care team, which may include your:
Involve your family and friends.
Click below for helpful tips on how your family and friends may help you manage your diabetes.